I caught a virus and never recovered – Part Three
The Horrible History of ME
 |
| The Horrible History of ME – illustrated by Amanda Francey The quality of life for those with ME is exactly the same as it was generations ago. |
It has been almost eight years since I caught a virus and never recovered, and I completely empathise with this growing group of COVID-19 “Long Haulers”.
The only surprising aspect of this post-viral “second act” of COVID-19, is the reaction by various media outlets and some “medical experts” describing this phenomenon as puzzling, baffling or mysterious, as though young, healthy people not recovering from a virus is something new, or unique to SARS-CoV-2.
If you’re a COVID-19 “Long Hauler” reading this, I bet you have spent some time wondering why – in 2021 – doctors seem either dismissive or baffled by your relapsing multitude of symptoms, lasting month after month, and nobody’s the wiser as to why you’re still too sick to resume a normal life.
Currently, there are no scientifically proven treatments that will return you to the normal, fully functioning human that you once were pre-COVID. However, careful pacing with decent rest periods between physical or cognitive activities, will give you a fighting chance. A subset of Long COVID will have a delayed recovery, but they will eventually fully recover. If you’re going to recover, it will most likely happen within the first year or two. But the more you push your energy deprived cells, the deeper the hole you may dig for yourself, which can lead to longer term or permanent disability.
Why is it a mystery, roughly ten percent of the population don’t fully recover from some viruses? And, more importantly, why are there no biomarkers or biomedical treatments for Myalgic Encephalomyelitis, when it has been classified as a neurological disorder by the World Health Organisation (WHO) since 1969?
There are several reasons why, and they are all unforgivable…
Starting with, medical misogyny and gender inequality, to the more malevolent motive by a faction of UK’s medical establishment falsifying the WHO’s international guidelines and wrongfully reclassifying ME as “psychological fatigue”, to the discredited PACE Trial and the recent hijacking attempt of millions more “long haulers” by psychiatrists. Throughout this article, I will touch on how these factors will affect people with Long COVID, concluding with what we should do about it.
Prior to proper scanning technology, Multiple Sclerosis (MS) was originally thought to be a man’s disease because historically women who presented with MS symptoms were automatically diagnosed with hysteria. Medical research now reveals MS is three or four times more common among women.
The above quote is from Cohut’s article The controversy of “female hysteria” published in Medical News Today. Mentioned in the article was a perfect example of this, The Yellow Wallpaper written by brilliant American writer Charlotte Perkins Gilman. The short story takes the form of a secret journal of Gilman’s own agonising experience. In her diary she wrote she was diagnosed with a “nervous depression, with slight hysterical tendency” by her husband, a physician of “high standing”. He prescribed the fashionable “radical rest” treatment of the era designed to tame modern women from wanting other things like an education, or in her case, a professional writing career.
According to the late Dr Stephen Straus, women could avoid these woes if only they stuck to homemaking and raising children instead of this unachievable ambition so often mentioned in medical texts, authored mostly by pompous middle-aged men. But more on Straus later.
On the other hand, if the woman was a dedicated and attentive mother, she was blamed for her child’s asthma. During the 1930s-50s asthma was believed to be a psychosomatic condition caused by a person’s relationship with their mother. Gasping for oxygen was apparently an unconscious suppressed impulse to cry for the mother’s attention, because the mother had overly affectionate tendencies. The treatment was to remove the child from their mother.
Now we know Long COVID also predominately affects working-age women, we need to make sure history doesn’t repeat. And we need to monitor the media and call them out if they start using stigmatising words like “Yuppie Flu” or “Mass Hysteria”.
Forbes and BBC News have at least read and reported the science of Long COVID, focusing more on the physical symptoms such as, breathlessness, fatigue, muscle pain, brain fog and an abnormal immune response.
Of course anxiety or depression can be additional, but they’re more likely to be a secondary consequence rather than causation. I imagine anyone who has felt physically rotten for months with no answers or treatments, and no end date to this Long COVID nightmare, could be feeling some anxiety or depression.
This is why biomedical research grants need to take preference over psychological therapies, because this is predominately a physical condition. Biomedical research is the only way forward, but…
It wasn’t until 1956, Dr. A. Melvin Ramsay formally coined Sir Donald Acheson’s selected name for the disease Myalgic Encephalomyelitis in a paper describing the 1955 epidemic among staff at Royal Free Hospital in London. Dr. Ramsay investigated ME for more than 30 years and published the Ramsay Definition of ME in 1986.
In the WHO’s International Classification of Diseases, Myalgic Encephalomyelitis, post-infectious encephalomyelitis and other encephalomyelitis diseases were classified as neurological disorders since 1969 (ICD-8), under the same code 323. However, after an outbreak of ME in Incline Village, Nevada in 1984, Chronic Fatigue Syndrome (CFS) was proposed in 1987 by the Centers of Disease Control (CDC).
The following year, the Holmes definition (also called the 1988 CDC criteria) was when “Chronic Fatigue Syndrome” became the formal title, which has trivialised this life-altering condition with its common use since.
Then in 1991 came the disastrous Oxford Criteria, which took the psychologising of this debilitating condition to a whole new level. Lead-author Professor Michael Sharpe ignored all other physical symptoms and biomedical findings and focused predominantly on psychological and lifestyle factors.
The Oxford Criteria has since been widely criticised by researchers, advocacy groups and the National Institutes of Health (NIH) as being severely flawed. It was so broad the entry criteria could have resulted in a selection of study participants with other fatiguing illnesses. “For every 15 patients selected under Oxford criteria, 14 will be false positives when compared to the more recent Canadian Consensus Criteria.” Hardly surprising considering depression was included and specialist testing or investigations for other diseases were strongly discouraged. Most likely to save costs.
Moreover, the hallmark symptom of ME, post-exertional malaise (PEM) was not even mentioned in the Oxford Criteria, and no physical symptoms were even required.
Then in 1994, PEM was added to the Fukuda Criteria, but as it was not mandatory it ran the risk of doctors misdiagnosing the wrong patient group with ME and muddying the waters for research results.
Stephen Straus, the physician I mentioned earlier, who believed women could avoid the woes of ME/CFS if only they were less ambitious, became heavily involved in the Fukuda Criteria. Straus carried a considerable influence globally, and had actively discredited the biological grounds of ME during the time he worked for the NIH.
As you will see, written in the letter below, the desirable outcome to “evaporate” Myalgic Encephalomyelitis as a distinct disease was actioned by these members of NIH - National Institute of Allergy & Infectious Diseases (NIAID) and CDC. A letter obtained by ME advocate Craig Maupin via a FOIA request (Freedom of Information Act request), was sent from NIH’s Dr. Stephen Straus to CDC’s Dr. Keiji Fukuda in 1994.
Below is an extract from Thirty Years of Disdain – How a Group of Psychiatrists Buried ME, by Mary Dimmock and Matthew Lazell-Fairman.
Betraying the unspoken intent behind the Fukuda definition, Dr. Straus made the following points:
Craig Maupin had endured decades living with this debilitating illness since he was 17. I wanted to reach out to Craig a few months after I began researching and writing my three part story, but sadly Craig passed away only a month prior to this, at the age of 49 in August, 2019. Craig is one of many patients that has deeply motivated me to continue raising awareness of the injustice of ME.
The combination of the name change to CFS and 1980s-1990s vague diagnostic criteria, paved the way to make ME disappear and for psychiatry to take over with Chronic Fatigue Syndrome.
And here’s another quote from Sharpe revealing his concern about costs in the same 1991 British Medical Bulletin article: Psychiatric Management of Post Viral Fatigue Syndrome.
No doubt Sharpe’s concern over costs were due to his links with the medical insurance industry, including Unum Group formally known as UnumProvident. In 1994, Unum reported that no other disease surpassed the rate of increase of ME/CFS. In order of insurance costs, ME/CFS came second in the list of the five most expensive chronic conditions, being three places ahead of AIDS. Under the guise of a Chronic Fatigue Syndrome Management Program, Unum set out to discredit the condition.
UNUM’s “CFS Management Plan” states: “UNUM stands to lose millions if we do not move quickly to address this increasing problem.”
Unum, along with many other major insurance companies known to be involved in ME/CFS claims, such as Norwich Union, uses Swiss Re as re-insurer, whose “CFS experts” include Michael Sharpe. And they all use the same group of psychiatrists to inter-refer claimants with ME/CFS.
Insurance companies have saved millions, if not billions, in the past, leaving desperately ill ME patients to fend for themselves, and they would have no qualms about doing it all over again with Long COVID. In fact, Sharpe has started the ball rolling with a persuasive presentation alleging a subset of Long COVID patients are not suffering from a physical condition, but a psychosocial or psychosomatic disorder to major global reinsurer, Swiss Re. But more on Sharpe’s recent wickedness later.
“Sir” Simon Wessely – another physician of “high standing” – was lecturing in British Columbia, while Dr Byron Hyde watched on appalled. Wessely had hundreds of staff and physicians laughing themselves silly at the expense of a highly vulnerable and incredibly sick patient group, which had devastating consequences:
The next morning I left by car with my crew and arrived in Kelowna British Columbia that afternoon. We were staying at a patient’s house who had severe M.E. with dysautanomia and was for all purposes bed ridden or house bound most of the day. That morning she had received a phone call from her insurance company in Toronto. (Toronto is approximately 2742 miles from Vancouver). The insurance call was as follows and again I paraphrase: “Physicians at a University of British Columbia University have demonstrated that there is no pathological or physiological basis for M.E. or CFS. Your disability benefits have been stopped as of this month. You will have to pay back the funds we have sent you previously. We will contact you shortly with the exact amount you owe us.”
That night I spoke to several patients or their spouses came up to me and told me they had received the same message. They were in understandable fear.
What is important about this story is that at that meeting it was only Dr Wessely who was speaking out against M.E. and CFS and how … were the insurance companies in Toronto and elsewhere able to obtain this information and get back to the patients within a 24 hour period if Simon Wessely was not working for the insurance industry… I understand that it was also the insurance industry who paid for Dr Wessely’s trip to Vancouver.” ~ Byron Hyde, MD (written in 2011)
In September 2001, the WHO issued a statement effectively repudiating Wessely’s classification of ME in the WHO guide and on the website, which had been manipulated by the Institute of Psychiatry at King’s College Hospital, London, and the Department of Psychiatry at Oxford University, where Wessely, Sharpe and a number of “psychosomatic ME” promotors are based.
One of the worst repercussions of this medical injustice, has seen children ripped from the arms of their loving parents. The children are placed into the care of ignorant healthcare professionals, who then coerce them into harmful psychiatric therapies at a devastating cost to the child’s health.
In November 2001, assembled on the stairs above, you’ll see some of the psychiatrists who are responsible for gaslighting, stigmatising and, since the internet, trolling patients for decades. I took a page from Brian Hughes’ The Science Bit book and edited the image to blur them and remove their names out of courtesy. I also wiggled them a little purely for self amusement.
Oh and this conference at Woodstock, Oxford was payed for by UK’s Department for Work and Pensions (DWP).
Over a hundred researchers, scientists, professors and doctors signed an open letter criticising the deep flaws in the PACE Trial. This was only after a lengthy and expensive legal battle from another Freedom of Information request, by ME patient Alem Matthees, to release the PACE Trial research raw data.
Below I’ve included an extract from an article from ME/CFS awareness day website, may12th.org.au, detailing the great lengths these PACE Trial authors went to in their desperate attempt to keep that data concealed from public and scientific scrutiny.
Reanalysis of the methodology found numerous flaws, including that during the study, they had changed the thresholds for what counted as recovery. Some patients who were still sick were also counted as recovered. A reanalysis of the data released to Alem brought to light that the claimed recovery rate in the 2011 PACE paper was between 3 and 7 per cent, instead of 22 per cent, questioning the validity of recommendations of CBT and GET as treatments for ME/CFS.”
When David Tuller, DrPH, public health journalist at UC Berkeley’s Center for Global Public Health, visited Australia in 2018, he made a special trip to Western Australia to visit Alem to congratulate and to thank him on behalf of millions of ME patients around the world. Tuller was saddened when he realised Alem’s health had declined dramatically since the 2016 tribunal.
Still today Alem’s health is very severe. His mother wrote in this story Alem’s life now consists of lying in bed 24 hours a day. He cannot leave the room. He wears an eye mask as he’s sensitive to light. He has ear plugs as he’s sensitive to sound. The room is darkened and he can no longer speak, read, watch TV or listen to the radio.
Criticisms of the PACE Trial, other than altering assessment thresholds (an obvious no-no), include the use of the appalling Oxford Criteria to recruit a patient cohort with various fatiguing illnesses, and the investigators contaminating the results to promote their therapy as successful to the patients they were studying.
The PACE Trial dominated health guidelines for ME in the UK, US, Canada, Australia and other countries. This impacted the lives of millions of patients worldwide in a negative way. At best, GET and CBT were counter-productive. At worst, they caused significant disability and irreversible deterioration. This was due to the patients being coerced into pushing past their limited capacity by ignorant physicians who hadn’t any medical training on the impaired energy system in patients with ME and the dangers of triggering a debilitating exacerbation of symptoms.
These three young women (pictured below), might still be here today if it weren’t for decades of biomedical research neglect and funding mostly funnelled into psychiatric research. Sharpe, Wessely and their colleagues were meant to be supporting ME patients, instead, they ridiculed them in front of impressionable medical peers, leading to catastrophic harm and unforgivable medical ignorance at an international level.
Despite GET and CBT being “quietly removed” from the US Centers of Disease Control list of recommendations in 2017, these harmful and grossly outdated treatments remain in both Australian and UK health guidelines for general practitioners while draft updates are pending feedback review.
Thankfully, UK’s draft update of their medical guidelines for ME/CFS released in November last year, pulled the plug on Graded Exercise Therapy and Cognitive Behavioural Therapy.
UK’s NICE guidance draft also specifically warned against the Lightning Process, Neurolinguistic Programming, Gupta and Life Coaching claiming to cure your physical illness. They’re more likely to make you much worse.
Unfortunately, the updated UK guidelines release date has been postponed from April until August this year due to the overwhelming feedback. ME patients and advocacy groups have already noticed the same group of UK psychiatrists responsible for the PACE Trial continue to oppose these new guidelines and allege NICE have been bullied into making these changes by “militant” patient groups. Yes, they do love the word “militant” to describe an incredibly sick patient group, mostly housebound and/or bed-bound thanks to being prescribed GET!
Oh and Sharpe and Wessely also love whinging loudly in bold letters about being silenced and facing death threats. Laughable in view of how physically disabled we are. The PACE Trial Freedom of Information Act Tribunal in 2015 found no death threats, and the only evidence of harassment was nothing more than a harmless heckle. Either these psychiatrists have grossly exaggerated their claims or they have paranoid delusions driven by subconscious guilt, which has led them to x-ray their mail and install panic buttons. A bit over the top considering our much limited energy and mobility.
These Pro-PACE Trial professors are in influential positions and continue to utilise their UK-media-mates, who carry on blindly echoing GET/CBT propaganda. It’s historically reminiscent and quite disturbing how these old physicians of “high standing” continue to dismiss all past and present international ME research showing: neurological impairments using neuroimaging techniques; reduced oxygen consumption and capacity to produce energy on demand using the two day cardiopulmonary exercise tests (CPETs); cellular mitochondrial abnormalities and defective calcium ion channel receptors predominantly affecting the brain, spinal cord, pancreas and stomach.
On the slide titled “Social factors - The media”, Sharpe accused Guardian journalist, George Monbiot, of super-spreading Long COVID just by writing about it. Monbiot had never heard of Michael Sharpe prior to this bizarre allegation, so he did a little digging and fought back with another article as well as this short news segment uncovering the medical misogyny and great harms psychiatry have caused patients with ME over the past three decades.
The best thing Sharpe has ever done for our community was give us George Monbiot, a brilliant and articulate ally for ME and Long COVID.
Sadly, it has taken a pandemic, and millions more suffering, for ME to finally be noticed. Countries worst hit by COVID-19 will be followed by a tsunami of post-COVID disability, which will likely contribute to the largest economic disaster we’ve ever seen, if health departments don’t take action now.
The only way forward is for governments to make a substantial financial commitment to fast-track research, and update physician education to counter the injustice based on decades of woefully underfunded biomedical research into post-viral neuroimmune diseases.
As grim as this horrid pandemic has been, there has been something positive come from it. Long COVID and ME advocacy groups have joined forces, not only supporting each other due to the void in medical care, but also advocating together. #MEAction and Body Politic – a patient-led organisation for Long COVID – have written letters to US’s National Institute of Health (NIH), asking them to prioritise funding for research that build on prior ME/CFS and related research in their investigation of Long COVID.
Why reinvent the wheel, when we already have valuable information and resources to build a clearer picture? This will save time, money and resources, which will enable ALL of us to regain enough health and functionality to return to school, work or caring for our family. I don’t know a single person in our joint community who wish to spend the rest of their life barely existing off benefit scraps. More than anything, we want the opportunity to “experience life” again.
If ME has been classified as a neurological disorder by the WHO since 1969, where have all the neurologists been for ME patients over the last 50 years? Out of all the “ologists” patients are referred to, neurologists have been the least supportive of our patient group. Most neurologists simply don’t want to treat us.
Not only should medical students and general practitioners be educated in ME and Long COVID, there needs to be training modules for neurologists, immunologists, cardiologists, gastroenterologists, endocrinologists, rheumatologists and physiotherapists. This might be predominately a neuroimmune disease, but also impacts multiple bodily systems, where other specialists will be required.
Over the last couple of years we have seen more positive research for ME than in previous decades. Funding is still appallingly low and is mostly raised by advocacy groups, patients and their families, but at least government financed grants have finally taken a step in the right direction, biomedical research.
UK’s Medical Research Council and the National Institute of Health Research recently funded £3.2 million for a large DNA study, DecodeME, to investigate DNA profiles of people with ME and CFS in comparison with healthy controls.
Australia’s NHMRC are investing $3.3 million (AU) in medical research for 2020-21 to improve the understanding of ME. This amount will be split over three successful grant applicants, to fund their biomedical research projects including: investigating stem cells and screening drugs for treatments; expanding on Griffith University’s calcium ion channel research, recognising biomarkers and developing diagnostic tests; and exploring the energy metabolism and mitochondrial function.
Another exciting development in Australia, Emerge announced they’ve been awarded a $1 million (AU) grant, funded by the Mason Foundation, to establish the first Australian ME biobank and patient registry. Emerge have partnered with Solve M.E. (based in the US) to help create the largest possible database. You+ME registry is now open for Australians.
All of this research is promising, however, it will take some time until effective treatments become available for ME and Long COVID patients. While we wait, we must look after ourselves to prevent further deterioration.
The most important thing you can do is pace your physical and cognitive activities with rest breaks in between. It’s tempting to push through, but if you have PEM, it can be harmful to push your body – or your brain – to do something when your energy system is running on empty.
#MEAction started a fantastic campaign to share with “COVID Long Haulers”. If you suffer from post-exertional malaise or post-exertional symptom exacerbation please watch this video:
The ME Association in the UK have written a statement on exercise in ME/CFS and Long COVID, along with some helpful activity management and information. It’s important to note, the ME Association are not against exercise, but warn against inflexible graded exercise or activity, as this can be harmful.
You can also find information on pacing from Physios for ME which includes a 15 minute film about activity and energy management. Some people find Heart Rate Monitoring can help accurately pace their daily activity and monitor their body’s response to exertion.
As more research emerges, we must stay alert and pushback any psychiatrists or physicians of “high standing” whenever they try to perpetuate their pseudoscientific beliefs to government agencies or insurance companies in the attempt to hijack our biomedical condition for their own agenda. We need to continue writing letters to editors, educating misinformed media as well.
While Long COVID and ME/CFS may have some differences, it’s important we stick together.
A special thank you to Herman Jan Couwenberg, best known as Dutch cartoonist Djanko for allowing me to feature their clever cartoon near the beginning of this final part to my story. The first two parts are a personal account of my life with ME.
Part one goes back almost eight years, to when it all began and the triggers that led me down the rabbit hole of chronic illness.
Part two describes my current life – seven years later in the midst of a pandemic – doing my best to articulate the gravity of this illness.
To conclude, I’d like to leave you with this brief but spectacular take on advocating for people with chronic illnesses…
 |
| Illustrated by Herman Jan Couwenberg, best known as Dutch cartoonist Djanko. The above cartoon was created in 2020, when the media saw Long COVID as a shiny new thing, ignoring decades of post-viral illnesses ruining millions of lives. However, it's important to note, many Long COVID patients are experiencing very little support or understanding by their doctors. |
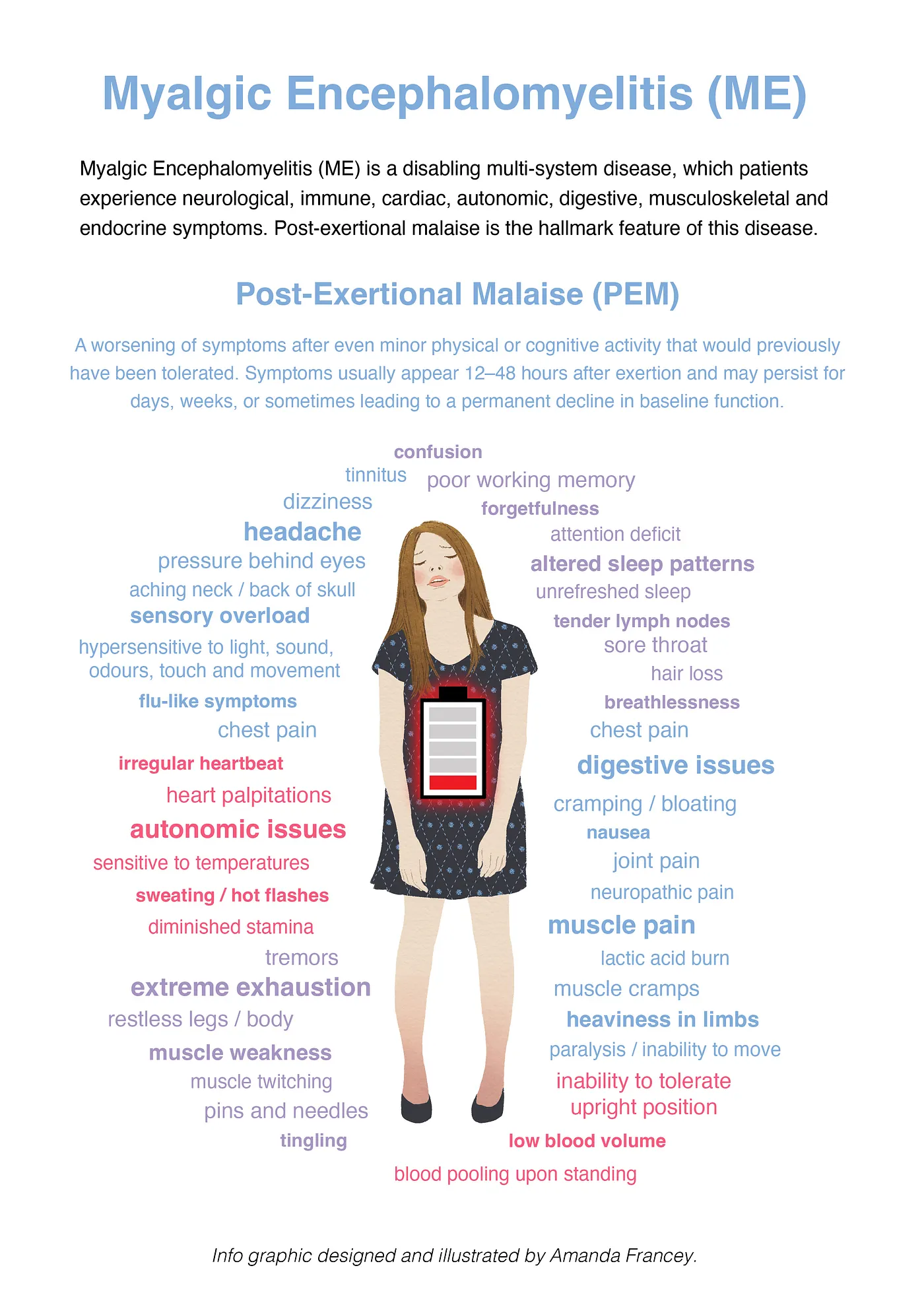
While damage to the heart, lungs or other organs can be chalked up as being a direct consequence of COVID-19 in a subset of patients, many of these long lasting symptoms affecting the brain, muscles, digestive, immune, cardiac and metabolic systems are remarkably similar to Myalgic Encephalomyelitis (ME), also referred to as Chronic Fatigue Syndrome (CFS), or the umbrella term ME/CFS.
If your symptoms worsen after physical or cognitive exertion, this phenomenon is called post-exertional malaise (PEM) – or post-exertional symptom exacerbation – which is the hallmark feature of ME. This exacerbation of symptoms can be triggered immediately after an activity, but is often delayed by hours or days and is disproportionate to the level of the activity.
Over seventy percent of ME patients report having a sudden onset of chronic symptoms after an acute viral infection and there are historic reports of ME clusters of epidemic proportions after viral outbreaks. ME can also be slow onset triggered by multiple viruses or an unknown origin and be equally as devastating or tragic.
If your symptoms worsen after physical or cognitive exertion, this phenomenon is called post-exertional malaise (PEM) – or post-exertional symptom exacerbation – which is the hallmark feature of ME. This exacerbation of symptoms can be triggered immediately after an activity, but is often delayed by hours or days and is disproportionate to the level of the activity.
Over seventy percent of ME patients report having a sudden onset of chronic symptoms after an acute viral infection and there are historic reports of ME clusters of epidemic proportions after viral outbreaks. ME can also be slow onset triggered by multiple viruses or an unknown origin and be equally as devastating or tragic.
 |
| Myalgic Encephalomyelitis / Chronic Fatigue Syndrome is NOT Chronic Fatigue |
If you’re a COVID-19 “Long Hauler” reading this, I bet you have spent some time wondering why – in 2021 – doctors seem either dismissive or baffled by your relapsing multitude of symptoms, lasting month after month, and nobody’s the wiser as to why you’re still too sick to resume a normal life.
Currently, there are no scientifically proven treatments that will return you to the normal, fully functioning human that you once were pre-COVID. However, careful pacing with decent rest periods between physical or cognitive activities, will give you a fighting chance. A subset of Long COVID will have a delayed recovery, but they will eventually fully recover. If you’re going to recover, it will most likely happen within the first year or two. But the more you push your energy deprived cells, the deeper the hole you may dig for yourself, which can lead to longer term or permanent disability.
Why is it a mystery, roughly ten percent of the population don’t fully recover from some viruses? And, more importantly, why are there no biomarkers or biomedical treatments for Myalgic Encephalomyelitis, when it has been classified as a neurological disorder by the World Health Organisation (WHO) since 1969?
There are several reasons why, and they are all unforgivable…
Starting with, medical misogyny and gender inequality, to the more malevolent motive by a faction of UK’s medical establishment falsifying the WHO’s international guidelines and wrongfully reclassifying ME as “psychological fatigue”, to the discredited PACE Trial and the recent hijacking attempt of millions more “long haulers” by psychiatrists. Throughout this article, I will touch on how these factors will affect people with Long COVID, concluding with what we should do about it.
Medical misogyny and gender inequality
Throughout history, women have not been believed to be reliable witnesses of their own bodies. This still happens today each time a doctor minimises or psychologises a woman’s health by not believing her lived experience.
In 1955, an infectious disease outbreak at the Royal Free Hospital in London, leaving hundreds of “long haulers” in its wake, was negligently labeled an outbreak of “mass-hysteria” by two male psychiatrists who hadn’t met a single patient. McEvedy and Beard wrote their hysteria hypothesis 15 years after the outbreak, based solely on the grounds that most people affected were women.“It wasn’t science. It was misogyny.” ~ George Monbiot, British author and columnist at The Guardian.
 |
| 1955 Royal Free Hospital London ME outbreak wrongfully labelled “Mass Hysteria” |
“For centuries, doctors readily diagnosed women with “hysteria” – an alleged mental health condition that explained away any behaviours or symptoms that made men… uncomfortable,” ~ Maria Cohut
According to the late Dr Stephen Straus, women could avoid these woes if only they stuck to homemaking and raising children instead of this unachievable ambition so often mentioned in medical texts, authored mostly by pompous middle-aged men. But more on Straus later.
Now we know Long COVID also predominately affects working-age women, we need to make sure history doesn’t repeat. And we need to monitor the media and call them out if they start using stigmatising words like “Yuppie Flu” or “Mass Hysteria”.
“It’s possible women have a different immune response to men.” ~ Dr Nazir Lone, consultant in critical care at the Royal Infirmary of Edinburgh, reported to BBC.
This is why biomedical research grants need to take preference over psychological therapies, because this is predominately a physical condition. Biomedical research is the only way forward, but…
Biomedical research resources and funding favours men
Currently, men get twice as much funding for diseases that mostly affect men.
In the US, Dr Arthur Mirin analysed the allocation of funds across diseases in 2020 and found the National Institutes of Health (NIH) gives a disproportionate share of its resources to diseases that primarily affect men with twice the funding.“ME is the lowest funded disease relative to disease burden by the NIH, and 75 percent of those afflicted are women,” wrote Dr Arthur A. Mirin. “Gender bias has been an ongoing issue in health care, examples being underrepresentation of women in health studies, trivialisation of women's physical complaints, and discrimination in the awarding of research grants,” he continued.
Evaporating ME as a distinct disease
The wrongful redefining Myalgic Encephalomyelitis as a “Fatigue Syndrome” was a deliberate intention to trivialise and dilute diagnostic criteria to focus solely on the vague and unmeasurable symptom “fatigue”.
Epidemic outbreaks and sporadic cases of ME have occurred since at least the 1930s, however it was likely occurring much earlier. The first recorded outbreak of ME was in 1934 in Los Angeles and was thought to be Atypical Polio. Iceland had similar ME outbreaks throughout the 1940s and 1950s, commonly known as Icelandic Disease.It wasn’t until 1956, Dr. A. Melvin Ramsay formally coined Sir Donald Acheson’s selected name for the disease Myalgic Encephalomyelitis in a paper describing the 1955 epidemic among staff at Royal Free Hospital in London. Dr. Ramsay investigated ME for more than 30 years and published the Ramsay Definition of ME in 1986.
In the WHO’s International Classification of Diseases, Myalgic Encephalomyelitis, post-infectious encephalomyelitis and other encephalomyelitis diseases were classified as neurological disorders since 1969 (ICD-8), under the same code 323. However, after an outbreak of ME in Incline Village, Nevada in 1984, Chronic Fatigue Syndrome (CFS) was proposed in 1987 by the Centers of Disease Control (CDC).
The following year, the Holmes definition (also called the 1988 CDC criteria) was when “Chronic Fatigue Syndrome” became the formal title, which has trivialised this life-altering condition with its common use since.
Then in 1991 came the disastrous Oxford Criteria, which took the psychologising of this debilitating condition to a whole new level. Lead-author Professor Michael Sharpe ignored all other physical symptoms and biomedical findings and focused predominantly on psychological and lifestyle factors.
The Oxford Criteria has since been widely criticised by researchers, advocacy groups and the National Institutes of Health (NIH) as being severely flawed. It was so broad the entry criteria could have resulted in a selection of study participants with other fatiguing illnesses. “For every 15 patients selected under Oxford criteria, 14 will be false positives when compared to the more recent Canadian Consensus Criteria.” Hardly surprising considering depression was included and specialist testing or investigations for other diseases were strongly discouraged. Most likely to save costs.
Moreover, the hallmark symptom of ME, post-exertional malaise (PEM) was not even mentioned in the Oxford Criteria, and no physical symptoms were even required.
Then in 1994, PEM was added to the Fukuda Criteria, but as it was not mandatory it ran the risk of doctors misdiagnosing the wrong patient group with ME and muddying the waters for research results.
Stephen Straus, the physician I mentioned earlier, who believed women could avoid the woes of ME/CFS if only they were less ambitious, became heavily involved in the Fukuda Criteria. Straus carried a considerable influence globally, and had actively discredited the biological grounds of ME during the time he worked for the NIH.
As you will see, written in the letter below, the desirable outcome to “evaporate” Myalgic Encephalomyelitis as a distinct disease was actioned by these members of NIH - National Institute of Allergy & Infectious Diseases (NIAID) and CDC. A letter obtained by ME advocate Craig Maupin via a FOIA request (Freedom of Information Act request), was sent from NIH’s Dr. Stephen Straus to CDC’s Dr. Keiji Fukuda in 1994.
Below is an extract from Thirty Years of Disdain – How a Group of Psychiatrists Buried ME, by Mary Dimmock and Matthew Lazell-Fairman.
Betraying the unspoken intent behind the Fukuda definition, Dr. Straus made the following points:
“My own sense is that a few years of use [with the Fukuda definition] in the field will once again verify that there is no demonstrable or reproducible differences between individuals who meet the full CFS criteria and those who can be said to suffer Idiopathic Chronic Fatigue. This would beg the question of whether additional revisions to the definition are warranted, or its entire abandonment. I predict that fatigue itself will remain the subject of considerable interest but the notion of a discrete form of fatiguing illness will evaporate. We would, then, be left with Chronic Fatigue that can be distinguished as Idiopathic or Secondary to an identifiable medical or psychiatric disorder. I consider this a desirable outcome”.
 |
| Letter from NIH-NIAID’s Dr. Stephen Straus to CDC’s Dr. Keiji Fukuda. |
The combination of the name change to CFS and 1980s-1990s vague diagnostic criteria, paved the way to make ME disappear and for psychiatry to take over with Chronic Fatigue Syndrome.
The hijacking of ME by psychiatrists with vested interests
Contributing to the evaporation of ME as a distinct disease, was the malignant movement by a group of influential professors in the UK. Principally among them are Professor Michael Sharpe and Sir Simon Wessely, both psychiatrists with links to the global insurance industry and close ties with UK’s Department for Work and Pensions (DWP).
“The use of extensive laboratory investigation may be psychologically harmful to the patient by reinforcing their beliefs about serious physical disease.” ~ Michael Sharpe.
“Even if shown to be beneficial (immunological) treatment is unlikely to be feasible on a wide scale because of cost.” – Michael Sharpe
UNUM’s “CFS Management Plan” states: “UNUM stands to lose millions if we do not move quickly to address this increasing problem.”
Unum, along with many other major insurance companies known to be involved in ME/CFS claims, such as Norwich Union, uses Swiss Re as re-insurer, whose “CFS experts” include Michael Sharpe. And they all use the same group of psychiatrists to inter-refer claimants with ME/CFS.
Insurance companies have saved millions, if not billions, in the past, leaving desperately ill ME patients to fend for themselves, and they would have no qualms about doing it all over again with Long COVID. In fact, Sharpe has started the ball rolling with a persuasive presentation alleging a subset of Long COVID patients are not suffering from a physical condition, but a psychosocial or psychosomatic disorder to major global reinsurer, Swiss Re. But more on Sharpe’s recent wickedness later.
“Sir” Simon Wessely – another physician of “high standing” – was lecturing in British Columbia, while Dr Byron Hyde watched on appalled. Wessely had hundreds of staff and physicians laughing themselves silly at the expense of a highly vulnerable and incredibly sick patient group, which had devastating consequences:
“Several years ago I was lecturing in British Columbia. Dr [Simon] Wessely was speaking and he gave a thoroughly enjoyable lecture on M.E. and CFS. He had the hundreds of staff physicians laughing themselves silly over the invented griefs of the M.E. and CFS patients who according to Dr Wessely had no physical illness what so ever but a lot of misguided imagination. I was appalled at his sheer effectiveness, the amazing control he had over the minds of the staid physicians….His message was very clear and very simple. If I can paraphrase him: “M.E. and CFS are non-existent illnesses with no pathology what-so-ever. There is no reason why they all cannot return to work tomorrow.
The next morning I left by car with my crew and arrived in Kelowna British Columbia that afternoon. We were staying at a patient’s house who had severe M.E. with dysautanomia and was for all purposes bed ridden or house bound most of the day. That morning she had received a phone call from her insurance company in Toronto. (Toronto is approximately 2742 miles from Vancouver). The insurance call was as follows and again I paraphrase: “Physicians at a University of British Columbia University have demonstrated that there is no pathological or physiological basis for M.E. or CFS. Your disability benefits have been stopped as of this month. You will have to pay back the funds we have sent you previously. We will contact you shortly with the exact amount you owe us.”
That night I spoke to several patients or their spouses came up to me and told me they had received the same message. They were in understandable fear.
What is important about this story is that at that meeting it was only Dr Wessely who was speaking out against M.E. and CFS and how … were the insurance companies in Toronto and elsewhere able to obtain this information and get back to the patients within a 24 hour period if Simon Wessely was not working for the insurance industry… I understand that it was also the insurance industry who paid for Dr Wessely’s trip to Vancouver.” ~ Byron Hyde, MD (written in 2011)
Hijacking the WHO logo to further the “psychosomatic ME” agenda
In an act of medical malfeasance, Wessely, and a faction of UK’s psychiatry establishment, knowingly falsified a section of the WHO guide. Wessely compiled a complete misrepresentation of ME by omitting numerous biological abnormalities and placing undue emphasis on lifestyle factors. He effectively changed the WHO’s classification of a physical neurological disorder to a mental health illness.
“I take no pleasure in, and set no store by, the suggestion that Professor Wessely effectively hijacked the WHO logo to give credence to his own view of ME as a mental illness. Nevertheless, I am uncomfortable that the professor does not appear to be doing his utmost to clear the air on this issue.” ~ Frederick R.P. Curzon
What other reason would Wessely change an internationally classified neurological disease, to a mental health illness, if it weren’t to further his own, and the insurance industry’s agenda?
Wessely’s falsifying of the WHO guide no doubt contributed to devastating ramifications for patients. Not only were disability support and services for ME patients in the UK wrongfully denied, some patients were forcibly removed from their homes and placed into psychiatric wards. Consequently, eighty percent of UK doctors still believe that ME or CFS is a mental health illness.One of the worst repercussions of this medical injustice, has seen children ripped from the arms of their loving parents. The children are placed into the care of ignorant healthcare professionals, who then coerce them into harmful psychiatric therapies at a devastating cost to the child’s health.
Malingering and Illness deception conference
 |
| Nothing to see here, just a few deceptive looking docs… malingering on some steps. |
Oh and this conference at Woodstock, Oxford was payed for by UK’s Department for Work and Pensions (DWP).
“Greatest medical scandal of the 21st century” – the PACE Trial
Instead of proper immune modulating medications, graded exercise therapy (GET) and cognitive behaviour therapy (CBT) have been the “go to” treatments for post viral conditions and ME/CFS, thanks to the debunked 2011 UK PACE Trial. It’s important to mention, the PACE Trial was also part-funded by the UK’s Department for Work and Pensions (DWP).
“This will emerge as one of the greatest medical scandals of the 21st century,” said Carol Monaghan, MP, during a parliamentary debate in Westminster. “A trial which claimed exercise helped the estimated 250,000 sufferers of the devastating illness, M.E., (myalgic encephalomyelitis) to recover was deliberately flawed to remove people from long-term benefits and reduce the welfare bill”.
Below I’ve included an extract from an article from ME/CFS awareness day website, may12th.org.au, detailing the great lengths these PACE Trial authors went to in their desperate attempt to keep that data concealed from public and scientific scrutiny.
“In March 2014, while quite unwell, Alem took his Freedom of Information request to Queen Mary University of London, initially in a polite letter. His request was refused, as were more than 30 other FOI requests from around the world. The university then spent a quarter of a million pounds (about $476,000 Australian dollars) fighting Alem’s more formal requests in the courts, which, in August 2016, eventually found in Alem’s favour.
Reanalysis of the methodology found numerous flaws, including that during the study, they had changed the thresholds for what counted as recovery. Some patients who were still sick were also counted as recovered. A reanalysis of the data released to Alem brought to light that the claimed recovery rate in the 2011 PACE paper was between 3 and 7 per cent, instead of 22 per cent, questioning the validity of recommendations of CBT and GET as treatments for ME/CFS.”
“Had they behaved as honest scientists and reported their original results, or released the data when asked, Alem could have harnessed his limited resources to other ends.” ~ David Tuller
The PACE Trial dominated health guidelines for ME in the UK, US, Canada, Australia and other countries. This impacted the lives of millions of patients worldwide in a negative way. At best, GET and CBT were counter-productive. At worst, they caused significant disability and irreversible deterioration. This was due to the patients being coerced into pushing past their limited capacity by ignorant physicians who hadn’t any medical training on the impaired energy system in patients with ME and the dangers of triggering a debilitating exacerbation of symptoms.
“It’s important to prevent harm that can occur from triggering post-exertional malaise.” – Dr Elizabeth Unger, Chief of CDC’s Chronic Viral Diseases.
 |
| From left: Sophia Mirza, Merryn Croft and Alison Hunter all died from very severe ME. |
Despite GET and CBT being “quietly removed” from the US Centers of Disease Control list of recommendations in 2017, these harmful and grossly outdated treatments remain in both Australian and UK health guidelines for general practitioners while draft updates are pending feedback review.
Thankfully, UK’s draft update of their medical guidelines for ME/CFS released in November last year, pulled the plug on Graded Exercise Therapy and Cognitive Behavioural Therapy.
NICE guidance went on to say GET “should NOT be presumed to be safe for those with this disabling and often neglected illness.”
Unfortunately, the updated UK guidelines release date has been postponed from April until August this year due to the overwhelming feedback. ME patients and advocacy groups have already noticed the same group of UK psychiatrists responsible for the PACE Trial continue to oppose these new guidelines and allege NICE have been bullied into making these changes by “militant” patient groups. Yes, they do love the word “militant” to describe an incredibly sick patient group, mostly housebound and/or bed-bound thanks to being prescribed GET!
 |
| Sharpe and Wessely looking silenced and utterly terrified. |
These Pro-PACE Trial professors are in influential positions and continue to utilise their UK-media-mates, who carry on blindly echoing GET/CBT propaganda. It’s historically reminiscent and quite disturbing how these old physicians of “high standing” continue to dismiss all past and present international ME research showing: neurological impairments using neuroimaging techniques; reduced oxygen consumption and capacity to produce energy on demand using the two day cardiopulmonary exercise tests (CPETs); cellular mitochondrial abnormalities and defective calcium ion channel receptors predominantly affecting the brain, spinal cord, pancreas and stomach.
The way they trumpet their pseudoscience nonsense every time biomedical research studies for ME reach mainstream headlines, is a pathetic and desperate attempt to cling onto their last strand of credibility.
And for the record, the reason why ME patients have fought so hard to have our illness rightfully recognised as physical, and not psychological, has nothing to do with prejudice. It’s because no amount of psychotherapy is going to return us to good health. Many of us have secondary depression or anxiety as a consequence of living with a highly debilitating and poorly understood disease. And don’t get me started on the large proportion of us suffering medical-gaslighting-induced PTSD no thanks to this same group of psychiatrists for stigmatising our disease by calling us “Those who have an imagined physical illness”, or worse “malingers” and “the underserving sick”.“I've had patients who met PTSD criteria... their trauma was their interaction with their physician. They came to the doctor with Chronic Fatigue Syndrome [ME]; they left with PTSD.” ~ Dr Nancy Klimas, Miami Herald, March 24, 2009.
We need biomedical treatments. And for that to happen, we need biomedical researchers. Not psychiatrists!
In Sharpe’s fourth-grade-style slideshow presentation to Swiss Re reinsurer, he warns “Beware of poor quality research with unclear denominators” while promoting the debunked PACE trial which is exactly that “poor quality research with unclear denominators”. I’ve highlighted some problematic points in my satirical but honest review of Sharpe’s presentation below:
We need biomedical treatments. And for that to happen, we need biomedical researchers. Not psychiatrists!
Psychiatrists attempting to hijack Long COVID
Why are psychiatrists still given a voice when Long COVID and ME/CFS are physical conditions?
Remember Sharpe and his cosy relationship with the insurance industry? Well he’s at it again, presenting at one of the largest global reinsurers, Swiss Re Group virtual Expert Forum on “secondary” impacts of COVID-19.In Sharpe’s fourth-grade-style slideshow presentation to Swiss Re reinsurer, he warns “Beware of poor quality research with unclear denominators” while promoting the debunked PACE trial which is exactly that “poor quality research with unclear denominators”. I’ve highlighted some problematic points in my satirical but honest review of Sharpe’s presentation below:
Then Sharpe includes a “single case study” Professor Garner – who had a “COVID like” illness and recovered by “thinking positively” and doing “military exercises”. One person tweeted a humorous response to this “single case study”:
Professor Garner messaged ME patient, Brendon, informing him within a few months of being ill, he was walking 5km per day, then began biking by October. During this time Garner claimed to have Long COVID, however going by the timeline, it was obvious he was well on his way to recovering anyway. Garner also claimed to have met the Canadian Consensus Criteria (CCC) for ME at seven months in November, the same month he was diving in the Caribbean during UK’s lockdown. His diving photos were conveniently deleted from Facebook around the time he was interviewed by BBC Breakfast about his “remarkable recovery”, but not before being screenshot and shared around twitter. There’s no hiding on the internet!
I may have “accidentally” slipped an extra slide in below:
“Jesus is depicted with long hair. I have long hair. I must be Jesus, right? 🤔🙄 N = 1 is not science. It’s an anecdote.”
Professor Garner messaged ME patient, Brendon, informing him within a few months of being ill, he was walking 5km per day, then began biking by October. During this time Garner claimed to have Long COVID, however going by the timeline, it was obvious he was well on his way to recovering anyway. Garner also claimed to have met the Canadian Consensus Criteria (CCC) for ME at seven months in November, the same month he was diving in the Caribbean during UK’s lockdown. His diving photos were conveniently deleted from Facebook around the time he was interviewed by BBC Breakfast about his “remarkable recovery”, but not before being screenshot and shared around twitter. There’s no hiding on the internet!I may have “accidentally” slipped an extra slide in below:
Where do we go from here?
Government health departments “worldwide” need to take responsibility for this massive injustice that has left ME patients without treatments, thus afflicting them with the poorest quality of life than most major diseases (some of which aren’t nearly as common). There are millions of us suffering year after year, decade after decade with no end in sight. And it looks as though ten million more are about to join us if this neglect continues.
If the NIH and health institutes around the world had given ME the biomedical funding they deserved over the last 30 years, I have no doubt patients with Long COVID would have diagnostic biomarkers to differentiate subgroups and offered effective treatments to not only manage symptoms, but prevent long-term or permanent disability so many ME patients suffer from today.Sadly, it has taken a pandemic, and millions more suffering, for ME to finally be noticed. Countries worst hit by COVID-19 will be followed by a tsunami of post-COVID disability, which will likely contribute to the largest economic disaster we’ve ever seen, if health departments don’t take action now.
The only way forward is for governments to make a substantial financial commitment to fast-track research, and update physician education to counter the injustice based on decades of woefully underfunded biomedical research into post-viral neuroimmune diseases.
As grim as this horrid pandemic has been, there has been something positive come from it. Long COVID and ME advocacy groups have joined forces, not only supporting each other due to the void in medical care, but also advocating together. #MEAction and Body Politic – a patient-led organisation for Long COVID – have written letters to US’s National Institute of Health (NIH), asking them to prioritise funding for research that build on prior ME/CFS and related research in their investigation of Long COVID.
Why reinvent the wheel, when we already have valuable information and resources to build a clearer picture? This will save time, money and resources, which will enable ALL of us to regain enough health and functionality to return to school, work or caring for our family. I don’t know a single person in our joint community who wish to spend the rest of their life barely existing off benefit scraps. More than anything, we want the opportunity to “experience life” again.
Hope on the horizon
A recent meeting between the American Academy of Neurology (AAN) science committee leaders and two of the US nation’s top NIH experts – Anthony Fauci and Walter Koroshetz – included a discussion focused on Long COVID and how it may advance better understanding of conditions like ME and CFS.
“We've been chasing myalgic encephalomyelitis and chronic fatigue syndrome without ever knowing what the etiologic agent was,” Fauci said. “Now we have an absolutely well-identified etiologic agent that should be very helpful now in getting us to be able to understand it. I hope we do; it's been mysterious to us for years. Maybe this will give us a chance at a breakthrough.”
“Chronic fatigue syndrome is a real mystery but, in that case, you never knew what the virus was,” Koroshetz said. “A lot of people said they had a viral illness and then they had this trouble. With COVID-19, we know when they had it, what it is, and we can actually try to trace the biology, and hopefully, get some clues that will help us understand and treat patients with post-acute COVID and potentially, people with chronic fatigue syndrome.”
“We've been chasing myalgic encephalomyelitis and chronic fatigue syndrome without ever knowing what the etiologic agent was,” Fauci said. “Now we have an absolutely well-identified etiologic agent that should be very helpful now in getting us to be able to understand it. I hope we do; it's been mysterious to us for years. Maybe this will give us a chance at a breakthrough.”
Then Koroshetz said something that made me feel hope and painfully betrayed at the same time.
“Neurologists have to play a really important role in trying to get at the bottom of this problem, because it really is in many instances, a neurological problem, along with dysautonomia, pain syndromes, abnormal sensations, and ‘big sleep troubles’ that linger for months after COVID is first diagnosed.”
Are neurologists going to drop the ball with Long COVID too?
With supporting statements like this from NIH’s Koroshetz and Fauci, our hope is no. It’s time for the neurology community to take post-viral neuroimmune diseases seriously.
Not only should medical students and general practitioners be educated in ME and Long COVID, there needs to be training modules for neurologists, immunologists, cardiologists, gastroenterologists, endocrinologists, rheumatologists and physiotherapists. This might be predominately a neuroimmune disease, but also impacts multiple bodily systems, where other specialists will be required.
Over the last couple of years we have seen more positive research for ME than in previous decades. Funding is still appallingly low and is mostly raised by advocacy groups, patients and their families, but at least government financed grants have finally taken a step in the right direction, biomedical research.
Research initiatives to study Long COVID
The US’s NIH has launched a $1.15 billion (US) initiative to study Long COVID over four years. While there was no mention of ME or CFS, they did point out that this research may improve our understanding of other chronic post-viral syndromes and autoimmune diseases. Let’s hope the money is spent wisely.
Prior to NIH’s announcement, Open Medicine Foundation (OMF) had already begun the only large-scale study of this kind, one that’s currently solely supported by private donors. In 2020, OMF secured a $1 million grant to launch the first year of an international, multi-year study across the five OMF funded Collaborative Research Centres (CRC). The aim of this study is to examine Post-COVID Syndrome transitioning to ME/CFS. OMF are actively working to raise an additional $2 million for years two and three of the study.
I’ve summarised Dr Tompkins’ recent statement during Open Medicine Foundation’s (OMF) Open House May 2021 event below:
Prior to NIH’s announcement, Open Medicine Foundation (OMF) had already begun the only large-scale study of this kind, one that’s currently solely supported by private donors. In 2020, OMF secured a $1 million grant to launch the first year of an international, multi-year study across the five OMF funded Collaborative Research Centres (CRC). The aim of this study is to examine Post-COVID Syndrome transitioning to ME/CFS. OMF are actively working to raise an additional $2 million for years two and three of the study.
I’ve summarised Dr Tompkins’ recent statement during Open Medicine Foundation’s (OMF) Open House May 2021 event below:
“There’s uncomplicated recovery, then there’s complicated, but eventual recovery, then there’s complicated and you never actually make it all the way back. So those are basically three different types of recoveries and you can associate those with genetics, proteomics and metabolomes.” ~ Ronald G. Tompkins, MD, ScD
Current ME/CFS research projects
US’s NIH also recently announced new resources for large-scale ME/CFS research. National Advisory Neurological Disorders and Stroke (NANDS) Council have approved two research tools mapMECFS – an interactive data pool – and searchMECFS – an interactive search tool – designed to advance ME/CFS research. These tools allow researchers to access and share data and biospecimens collected from people with ME/CFS who have volunteered to participate in clinical research:“Both of these tools include data sharing via centralised databases and biobanks for promoting communication between ME/CFS clinicians and researchers, as well as helping to advance progress in ME/CFS research. Scientists from all disciplines, including those who are studying the long-term effects of COVID-19, are invited to explore mapMECFS and searchMECFS to see how these tools can move their research projects forward.”
Australia’s NHMRC are investing $3.3 million (AU) in medical research for 2020-21 to improve the understanding of ME. This amount will be split over three successful grant applicants, to fund their biomedical research projects including: investigating stem cells and screening drugs for treatments; expanding on Griffith University’s calcium ion channel research, recognising biomarkers and developing diagnostic tests; and exploring the energy metabolism and mitochondrial function.
Another exciting development in Australia, Emerge announced they’ve been awarded a $1 million (AU) grant, funded by the Mason Foundation, to establish the first Australian ME biobank and patient registry. Emerge have partnered with Solve M.E. (based in the US) to help create the largest possible database. You+ME registry is now open for Australians.
All of this research is promising, however, it will take some time until effective treatments become available for ME and Long COVID patients. While we wait, we must look after ourselves to prevent further deterioration.
How to manage symptoms in the meantime
If a doctor tells you that your physically debilitating symptoms are due to being overly anxious about your health, please seek another opinion. You know your body and mental state better than they do.
First of all, you’ll need to take post-exertional malaise (PEM) more seriously than most doctors do. Due to the lack of medical education about the impaired energy system in a subset of those with Long COVID or ME, many doctors will likely minimise this as “fatigue” when there’s much more to it. Each major “PEM crash” I’ve had over the last eight years has deteriorated my health further. The more my health has declined, the more trivial, or disproportionate to the level of activity, my PEM inducing trigger has been.“Doctors need to be aware of symptoms that are very characteristic of ME, that if present, the doctors should stop, listen and pay attention to it. One of those is post-exertional malaise. With expenditure of energy, patients know if they cross a certain threshold, they’re going to pay a tremendous price for it. I know this is loosely termed as “fatigue”, but this is a much more specific form of fatigue and it’s not something that doctors are traditionally aware of or pay attention to.” ~ Dr Tompkins, OMF’s Open House May 2021 event.
#MEAction started a fantastic campaign to share with “COVID Long Haulers”. If you suffer from post-exertional malaise or post-exertional symptom exacerbation please watch this video:
Stop. Rest. Pace.
You can also find information on pacing from Physios for ME which includes a 15 minute film about activity and energy management. Some people find Heart Rate Monitoring can help accurately pace their daily activity and monitor their body’s response to exertion.
Final note
We need to continue fighting for research funding into the biological abnormalities and possible drug treatments for ME/CFS and Long COVID.As more research emerges, we must stay alert and pushback any psychiatrists or physicians of “high standing” whenever they try to perpetuate their pseudoscientific beliefs to government agencies or insurance companies in the attempt to hijack our biomedical condition for their own agenda. We need to continue writing letters to editors, educating misinformed media as well.
While Long COVID and ME/CFS may have some differences, it’s important we stick together.
Our voices are much stronger as a collective.
I hadn’t intended for part three of my story to be so long, but then I hadn’t imagined the whole world would have stopped due to a deadly pandemic, followed by a flood of “Long Haulers” in such a short space of time. I decided to extend part three for those with Long COVID in the hope it helps bring us all together and spread more awareness of both ME and LC during ME Awareness month.A special thank you to Herman Jan Couwenberg, best known as Dutch cartoonist Djanko for allowing me to feature their clever cartoon near the beginning of this final part to my story. The first two parts are a personal account of my life with ME.
Part one goes back almost eight years, to when it all began and the triggers that led me down the rabbit hole of chronic illness.
Part two describes my current life – seven years later in the midst of a pandemic – doing my best to articulate the gravity of this illness.
To conclude, I’d like to leave you with this brief but spectacular take on advocating for people with chronic illnesses…
. . . .









